- Clinical Study
- Fasting and Postprandial Hyperglycemia: Their Predictors and Contributions to Overall Hyperglycemia in Korean Patients with Type 2 Diabetes
-
Jaecheol Moon, Ji Young Kim, Soyeon Yoo, Gwanpyo Koh
-
Endocrinol Metab. 2020;35(2):290-297. Published online June 24, 2020
-
DOI: https://doi.org/10.3803/EnM.2020.35.2.290
-
-
6,909
View
-
201
Download
-
5
Web of Science
-
5
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Background
This study aimed to identify factors that affect fasting hyperglycemia (FHG) and postprandial hyperglycemia (PPG) and their contributions to overall hyperglycemia in Korean patients with type 2 diabetes mellitus (T2DM).
Methods
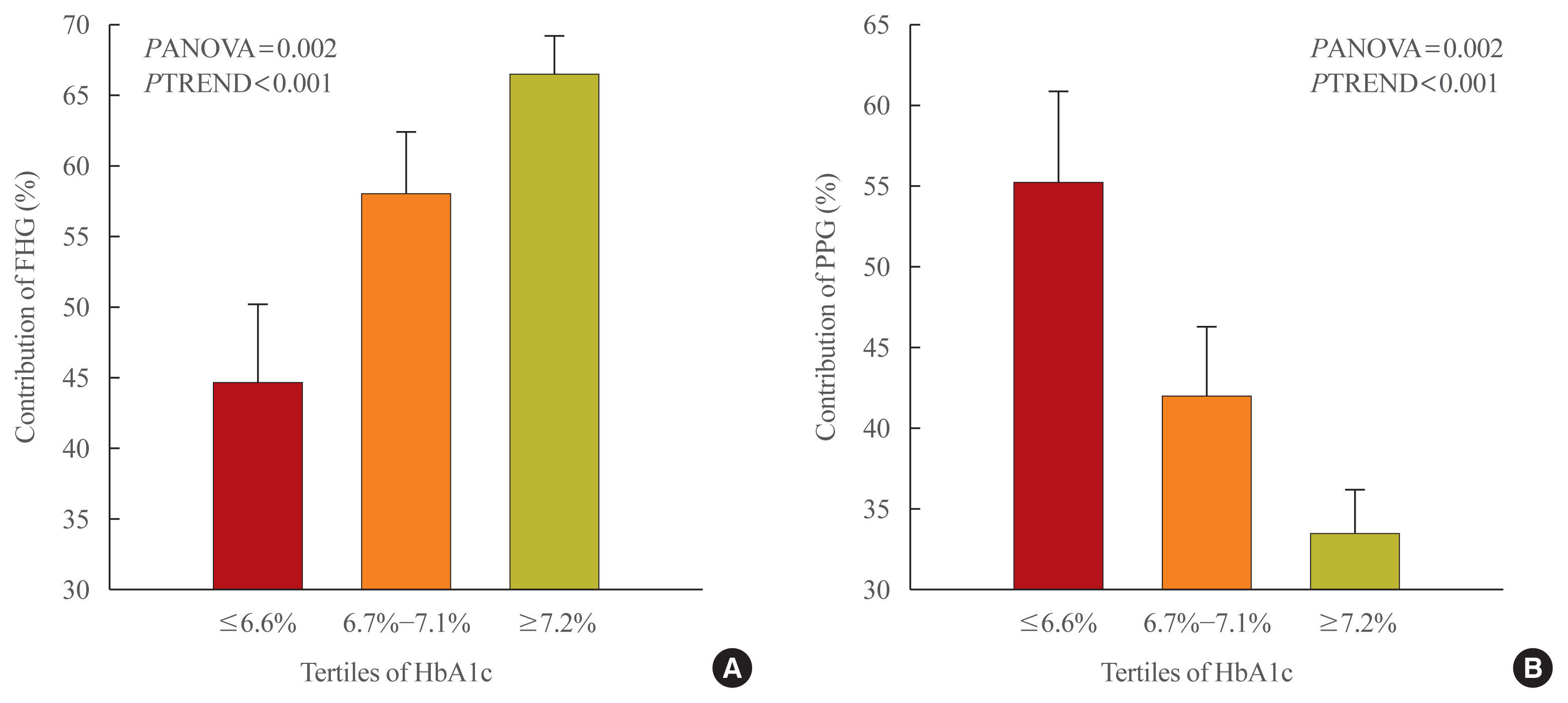
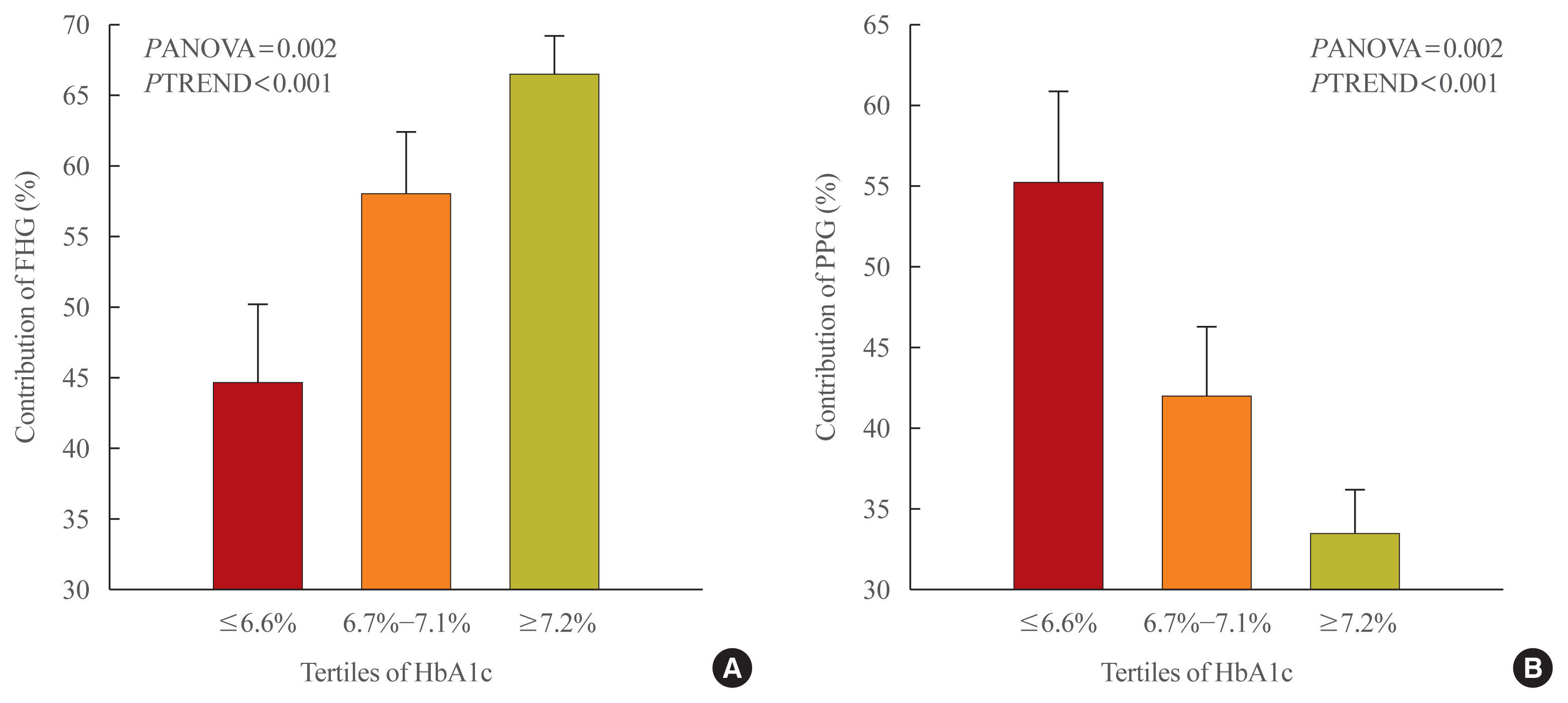
This was a retrospective study conducted on 194 Korean T2DM patients with 7-point self-monitoring blood glucose (SMBG) profiles plotted in 4 days in 3 consecutive months. We calculated the areas corresponding to FHG and PPG (area under the curve [AUC]FHG and AUCPPG) and contributions (%) in the graph of the 7-point SMBG data. The levels of glycated hemoglobin (HbA1c) were categorized by tertiles, and the contributions of FHG and PPG were compared.
Results
The relative contribution of FHG increased (44.7%±5.6%, 58.0%±4.4%, 66.5%±2.8%; PANOVA=0.002, PTREND <0.001), while that of PPG decreased (55.3%±5.5%, 42.0%±4.4%, 33.5%±2.8%; PANOVA=0.002, PTREND <0.001) with the elevated HbA1c. Multivariate analysis showed that HbA1c (β=0.615, P<0.001), waist circumference (β=0.216, P=0.042), and triglyceride (β=0.121, P=0.048) had a significant association with AUCFHG. Only HbA1c (β=0.231, P=0.002) and age (β=0.196, P=0.009) was significantly associated with AUCPPG.
Conclusion
The data suggested that in Korean T2DM patients, FHG predominantly contributed to overall hyperglycemia at higher HbA1c levels, whereas it contributed to PPG at lower HbA1c levels. It is recommended that certain factors, namely age, degree of glycemic control, obesity, or triglyceride levels, should be considered when prescribing medications for T2DM patients.
-
Citations
Citations to this article as recorded by  - Prospective study of the association between chronotype and cardiometabolic risk among Chinese young adults
Tingting Li, Yang Xie, Shuman Tao, Liwei Zou, Yajuan Yang, Fangbiao Tao, Xiaoyan Wu
BMC Public Health.2023;[Epub] CrossRef - Effects of mulberry twig alkaloids(Sangzhi alkaloids) and metformin on blood glucose fluctuations in combination with premixed insulin-treated patients with type 2 diabetes
Ziyu Meng, Chengye Xu, Haoling Liu, Xinyuan Gao, Xinyu Li, Wenjian Lin, Xuefei Ma, Changwei Yang, Ming Hao, Kangqi Zhao, Yuxin Hu, Yi Wang, Hongyu Kuang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - A new approach for investigating the relative contribution of basal glucose and postprandial glucose to HbA1C
Jing Ma, Hua He, Xiaojie Yang, Dawei Chen, Cuixia Tan, Li Zhong, Qiling Du, Xiaohua Wu, Yunyi Gao, Guanjian Liu, Chun Wang, Xingwu Ran
Nutrition & Diabetes.2021;[Epub] CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef
- Obesity and Metabolism
- Factors Associated with Glycemic Variability in Patients with Type 2 Diabetes: Focus on Oral Hypoglycemic Agents and Cardiovascular Risk Factors
-
Soyeon Yoo, Sang-Ouk Chin, Sang-Ah Lee, Gwanpyo Koh
-
Endocrinol Metab. 2015;30(3):352-360. Published online August 4, 2015
-
DOI: https://doi.org/10.3803/EnM.2015.30.3.352
-
-
3,918
View
-
47
Download
-
9
Web of Science
-
9
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader
- Background
The role of glycemic variability (GV) in development of cardiovascular diseases remains controversial, and factors that determine glucose fluctuation in patients with diabetes are unknown. We investigated relationships between GV indices, kinds of oral hypoglycemic agents (OHAs), and cardiovascular risk factors in patients with type 2 diabetes mellitus (T2DM). MethodsWe analyzed 209 patients with T2DM. The GV index (standard deviation [SD] and mean absolute glucose change [MAG]) were calculated from 7-point self-monitoring of blood glucose profiles. The patients were classified into four groups according to whether they take OHAs known as GV-lowering (A) and GV-increasing (B): 1 (A only), 2 (neither), 3 (both A and B), and 4 (B only). The 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was calculated using the Pooled Cohort Equations. ResultsGV indices were significantly higher in patients taking sulfonylureas (SUs), but lower in those taking dipeptidyl peptidase-4 inhibitors. In hierarchical regression analysis, the use of SUs remained independent correlates of the SD (β=0.209, P=0.009) and MAG (β=0.214, P=0.011). In four OHA groups, GV indices increased progressively from group 1 to group 4. However, these did not differ according to quartiles of 10-year ASCVD risk. ConclusionGV indices correlated significantly with the use of OHAs, particularly SU, and differed significantly according to combination of OHAs. However, cardiovascular risk factors and 10-year ASCVD risk were not related to GV indices. These findings suggest that GV is largely determined by properties of OHAs and not to cardiovascular complications in patients with T2DM.
-
Citations
Citations to this article as recorded by  - Prognostic value of longitudinal HbA1c variability in predicting the development of diabetic sensorimotor polyneuropathy among patients with type 2 diabetes mellitus: A prospective cohort observational study
Yun‐Ru Lai, Wen‐Chan Chiu, Chih‐Cheng Huang, Ben‐Chung Cheng, I‐Hsun Yu, Chia‐Te Kung, Ting Yin Lin, Hui Ching Chiang, Chun‐En Aurea Kuo, Cheng‐Hsien Lu
Journal of Diabetes Investigation.2024; 15(3): 326. CrossRef - Influence of dipeptidyl peptidase-4 inhibitors on glycemic variability in patients with type 2 diabetes: A meta-analysis of randomized controlled trials
Shangyu Chai, Ruya Zhang, Ye Zhang, Richard David Carr, Yiman Zheng, Swapnil Rajpathak, Miao Yu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Glycemic Variability in Subjects with Diabetes and Hypogonadism during Testosterone Replacement Treatment: A Pilot Study
Giuseppe Defeudis, Ernesto Maddaloni, Giovanni Rossini, Alfonso Maria Di Tommaso, Rossella Mazzilli, Paolo Di Palma, Paolo Pozzilli, Nicola Napoli
Journal of Clinical Medicine.2022; 11(18): 5333. CrossRef - New Insights into the Role of Visit-to-Visit Glycemic Variability and Blood Pressure Variability in Cardiovascular Disease Risk
Jin J. Zhou, Daniel S. Nuyujukian, Peter D. Reaven
Current Cardiology Reports.2021;[Epub] CrossRef - Prevalence of glycemic variability and factors associated with the glycemic arrays among end-stage kidney disease patients on chronic hemodialysis
Abdul Hanif Khan Yusof Khan, Nor Fadhlina Zakaria, Muhammad Adil Zainal Abidin, Nor Azmi Kamaruddin
Medicine.2021; 100(30): e26729. CrossRef - Dipeptidyl-Peptidase-IV Inhibitors, Imigliptin and Alogliptin, Improve Beta-Cell Function in Type 2 Diabetes
Xu Liu, Yang Liu, Hongzhong Liu, Haiyan Li, Jianhong Yang, Pei Hu, Xinhua Xiao, Dongyang Liu
Frontiers in Endocrinology.2021;[Epub] CrossRef - HbA 1C variability and hypoglycemia hospitalization in adults with type 1 and type 2 diabetes: A nested case-control study
Victor W. Zhong, Juhaeri Juhaeri, Stephen R. Cole, Christina M. Shay, Penny Gordon-Larsen, Evangelos Kontopantelis, Elizabeth J. Mayer-Davis
Journal of Diabetes and its Complications.2018; 32(2): 203. CrossRef - Glucose fluctuation and the resultant endothelial injury are correlated with pancreatic β cell dysfunction in patients with coronary artery disease
Makoto Murata, Hitoshi Adachi, Shigeru Oshima, Masahiko Kurabayashi
Diabetes Research and Clinical Practice.2017; 131: 107. CrossRef - Efficacy of lifestyle interventions in patients with type 2 diabetes: A systematic review and meta-analysis
Xiao-Li Huang, Jian-Hua Pan, Dan Chen, Jing Chen, Fang Chen, Tao-Tao Hu
European Journal of Internal Medicine.2016; 27: 37. CrossRef
- Obesity and Metabolism
- Apolipoprotein B Is Related to Metabolic Syndrome Independently of Low Density Lipoprotein Cholesterol in Patients with Type 2 Diabetes
-
Younghyup Lim, Soyeon Yoo, Sang Ah Lee, Sang Ouk Chin, Dahee Heo, Jae Cheol Moon, Shinhang Moon, Kiyoung Boo, Seong Taeg Kim, Hye Mi Seo, Hyeyoung Jwa, Gwanpyo Koh
-
Endocrinol Metab. 2015;30(2):208-215. Published online June 30, 2015
-
DOI: https://doi.org/10.3803/EnM.2015.30.2.208
-
-
4,580
View
-
46
Download
-
19
Web of Science
-
21
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader
- Background
Increased low density lipoprotein cholesterol (LDL-C) level and the presence of metabolic syndrome (MetS) are important risk factors for cardiovascular disease (CVD) in type 2 diabetes mellitus (T2DM). Recent studies demonstrated apolipoprotein B (apoB), a protein mainly located in LDL-C, was an independent predictor of the development of CVD especially in patients with T2DM. The aim of this study was to investigate the relationship between apoB and MetS in T2DM patients. MethodsWe analyzed 912 patients with T2DM. Fasting blood samples were taken for glycated hemoglobin, high-sensitivity C-reactive protein, total cholesterol, triglyceride (TG), high density lipoprotein cholesterol, LDL-C, and apoB. MetS was defined by the modified National Cholesterol Education Program Adult Treatment Panel III criteria. We performed a hierarchical regression analysis with apoB as the dependent variable. Age, sex, the number of components of MetS and LDL-C were entered at model 1, the use of lipid-lowering medications at model 2, and the individual components of MetS were added at model 3. ResultsSeventy percent of total subjects had MetS. ApoB level was higher in subjects with than those without MetS (104.5±53.3 mg/dL vs. 87.7±33.7 mg/dL, P<0.01) even after adjusting for LDL-C. ApoB and LDL-C were positively correlated to the number of MetS components. The hierarchical regression analysis showed that the increasing number of MetS components was associated with higher level of apoB at step 1 and step 2 (β=0.120, P<0.001 and β=0.110, P<0.001, respectively). At step 3, TG (β=0.116, P<0.001) and systolic blood pressure (β=0.099, P<0.05) were found to significantly contribute to apoB. ConclusionIn patients with T2DM, apoB is significantly related to MetS independently of LDL-C level. Of the components of MetS, TG, and systolic blood pressure appeared to be determinants of apoB.
-
Citations
Citations to this article as recorded by  - ApoB100 and Atherosclerosis: What’s New in the 21st Century?
Dimitris Kounatidis, Natalia G. Vallianou, Aikaterini Poulaki, Angelos Evangelopoulos, Fotis Panagopoulos, Theodora Stratigou, Eleni Geladari, Irene Karampela, Maria Dalamaga
Metabolites.2024; 14(2): 123. CrossRef - Association of apolipoproteins and lipoprotein(a) with metabolic syndrome: a systematic review and meta-analysis
Juan R. Ulloque-Badaracco, Ali Al-kassab-Córdova, Enrique A. Hernandez-Bustamante, Esteban A. Alarcon-Braga, Miguel Huayta-Cortez, Ximena L. Carballo-Tello, Rosa A. Seminario-Amez, Percy Herrera-Añazco, Vicente A. Benites-Zapata
Lipids in Health and Disease.2023;[Epub] CrossRef - Current Data and New Insights into the Genetic Factors of Atherogenic Dyslipidemia Associated with Metabolic Syndrome
Lăcramioara Ionela Butnariu, Eusebiu Vlad Gorduza, Elena Țarcă, Monica-Cristina Pânzaru, Setalia Popa, Simona Stoleriu, Vasile Valeriu Lupu, Ancuta Lupu, Elena Cojocaru, Laura Mihaela Trandafir, Ștefana Maria Moisă, Andreea Florea, Laura Stătescu, Minerva
Diagnostics.2023; 13(14): 2348. CrossRef - Apolipoprotein B compared with low-density lipoprotein cholesterol in the atherosclerotic cardiovascular diseases risk assessment
Federica Galimberti, Manuela Casula, Elena Olmastroni
Pharmacological Research.2023; 195: 106873. CrossRef - Circulating lipids and breast cancer prognosis in the Malmö diet and cancer study
Sixten Harborg, Thomas P. Ahern, Maria Feldt, Ann H. Rosendahl, Deirdre Cronin-Fenton, Olle Melander, Signe Borgquist
Breast Cancer Research and Treatment.2022; 191(3): 611. CrossRef - Metabolic disorders in patients with impaired glucose tolerance, with or without underlying ischaemic heart disease
Milena Brkić, Danijel Đekić, Jelena Jovanić, Goran Topić, Aleksandra Grbić, Tatjana Šutilović
Scripta Medica.2022; 53(3): 175. CrossRef - Genetics of Cholesterol-Related Genes in Metabolic Syndrome: A Review of Current Evidence
Sok Kuan Wong, Fitri Fareez Ramli, Adli Ali, Nurul ‘Izzah Ibrahim
Biomedicines.2022; 10(12): 3239. CrossRef - Prevalence of ApoB100 rs693 gene polymorphism in metabolic syndrome among female students at King Abdulaziz University
Rana A. Alghamdi, Maryam H. Al-Zahrani, Maha J. Balgoon, Nuha A. Alkhattabi
Saudi Journal of Biological Sciences.2021; 28(6): 3249. CrossRef - Local ablation of gastric cancer by reconstituted apolipoprotein B lipoparticles carrying epigenetic drugs
Chia-Lung Yang, Ying-Jui Chao, Hao-Chen Wang, Ya-Chin Hou, Caleb Gonshen Chen, Chia-Ching Chang, Yan-Shen Shan
Nanomedicine: Nanotechnology, Biology and Medicine.2021; 37: 102450. CrossRef - Cardiovascular Biomarkers of Obesity and Overlap With Cardiometabolic Dysfunction
Emily S. Lau, Samantha M. Paniagua, Shahrooz Zarbafian, Udo Hoffman, Michelle T. Long, Shih‐Jen Hwang, Paul Courchesne, Chen Yao, Jiantao Ma, Martin G. Larson, Daniel Levy, Ravi V. Shah, Jennifer E. Ho
Journal of the American Heart Association.2021;[Epub] CrossRef - The association of ecg TV1>TV6 phenomenon as electrophysiological sign of metabolic myocardial disorders with risk factors for ischemic heart disease in the population of 25–44 years
N. A. Kuzminykh, L. V. Shcherbakova, V. S. Shramko, D. V. Denisova, Yu. I. Ragino
Ateroscleroz.2021; 17(2): 22. CrossRef - Regulation of Apolipoprotein B by Natural Products and Nutraceuticals: A Comprehensive Review
Mohammad Bagherniya, Thomas P. Johnston, Amirhossein Sahebkar
Current Medicinal Chemistry.2021; 28(7): 1363. CrossRef - Apolipoprotein B and non-high-density lipoprotein cholesterol reveal a high atherogenicity in individuals with type 2 diabetes and controlled low-density lipoprotein-cholesterol
Liliana Fonseca, Sílvia Paredes, Helena Ramos, José Carlos Oliveira, Isabel Palma
Lipids in Health and Disease.2020;[Epub] CrossRef - Menopause-Associated Lipid Metabolic Disorders and Foods Beneficial for Postmenopausal Women
Seong-Hee Ko, Hyun-Sook Kim
Nutrients.2020; 12(1): 202. CrossRef - Lipoprotein A, combined with alanine aminotransferase and aspartate aminotransferase, contributes to predicting the occurrence of NASH: a cross-sectional study
Yu Zhang, He He, Yu-Ping Zeng, Li-Dan Yang, Dan Jia, Zhen-Mei An, Wei-Guo Jia
Lipids in Health and Disease.2020;[Epub] CrossRef - Novel and traditional lipid profiles in Metabolic Syndrome reveal a high atherogenicity
Sílvia Paredes, Liliana Fonseca, Laura Ribeiro, Helena Ramos, José Carlos Oliveira, Isabel Palma
Scientific Reports.2019;[Epub] CrossRef - Serum apolipoprotein B is associated with increased risk of metabolic syndrome among middle‐aged and elderly Chinese: A cross‐sectional and prospective cohort study
Rui Du, Xueyan Wu, Kui Peng, Lin Lin, Mian Li, Yu Xu, Min Xu, Yuhong Chen, Donghui Li, Jieli Lu, Yufang Bi, Weiqing Wang, Guang Ning
Journal of Diabetes.2019; 11(9): 752. CrossRef - The role of metabolism disorders, inflammation, myocardial injury in development chronic heart failure in metabolic syndrome patients
A. P. Roytman, T. A. Fedorova, E. A. Ivanova, A. V. Bugrov, V. V. Dolgov
Laboratornaya sluzhba.2018; 7(4): 5. CrossRef - Serum apoB levels independently predict the development of non‐alcoholic fatty liver disease: A 7‐year prospective study
Jinghua Wang, Wanlin Zhu, Shujun Huang, Lei Xu, Min Miao, Chenjiao Wu, Chaohui Yu, Youming Li, Chengfu Xu
Liver International.2017; 37(8): 1202. CrossRef - Comprehensive assessment of lipoprotein subfraction profiles according to glucose metabolism status, and association with insulin resistance in subjects with early-stage impaired glucose metabolism
Jie-Eun Lee, Se Hee Min, Dong-Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Kyong Soo Park, Hak Chul Jang, Soo Lim
International Journal of Cardiology.2016; 225: 327. CrossRef - Association of Serum Apolipoprotein B with the Increased Risk of Diabetes in Korean Men
Hyo Hee Lim, Oh Yoen Kim
Clinical Nutrition Research.2016; 5(3): 204. CrossRef
|